What Is the Lowest Oxygen Level Before Death?
Understanding Oxygen Levels at End-of-Life
It is difficult to define a single "lowest" oxygen level before death, as the dying process is a complex physiological decline involving multiple systems. However, critically low blood oxygen saturation (SpO2) is a significant indicator. A reading persistently below 80% without medical intervention is often associated with the final stages of life, but the rate of decline and other vital signs are equally important.
This information is sensitive and is intended for educational purposes to help families and caregivers understand the signs of physiological decline.
Critical Oxygen Level Ranges and Their Implications
The following chart outlines general SpO2 thresholds and their clinical significance in the context of end-of-life care:
| SpO2 Range | Clinical Significance & Symptoms |
|---|---|
| 90% - 94% | Low (Hypoxemia). Requires medical attention. May cause shortness of breath, rapid heart rate. |
| 85% - 89% | Severely Low. Risk of organ damage. Confusion, restlessness, and significant respiratory distress are common. |
| 80% - 84% | Critically Low. Often leads to loss of consciousness, severe confusion, and cyanosis (bluish skin). |
| 70% - 79% | Pre-Terminal. Frequently observed in the final 24-48 hours of life. The body's vital functions are slowing down. |
⚠️ Important Note: These ranges are general guidelines. Some individuals with chronic lung conditions may tolerate slightly lower levels, while others may decline more rapidly at higher levels.
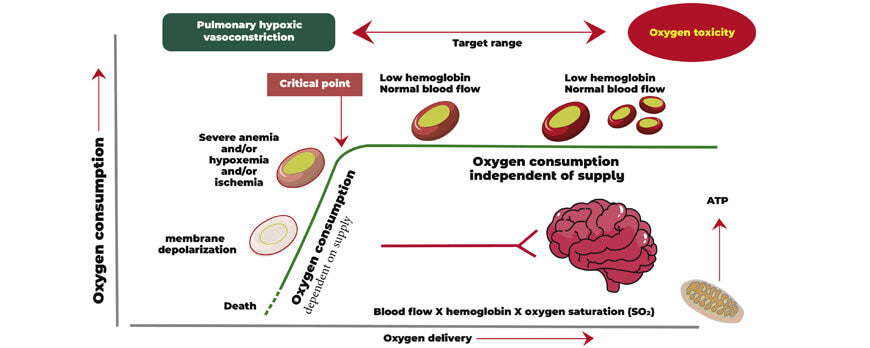
Key Physiological Factors in the Final Stages
A low oxygen level rarely occurs in isolation. The dying process involves the simultaneous failure of multiple systems:
-
Rate of Decline: A rapid drop in SpO2 is often more significant than a single very low number. A slow, gradual decline may be part of a longer-term process.
-
Blood Pressure: A significant and sustained drop in blood pressure (hypotension) is a strong concurrent sign that the heart is struggling to circulate blood.
-
Level of Consciousness: As oxygen levels fall, confusion, drowsiness, and eventually unresponsiveness are common. This is due to the brain not receiving enough oxygen.
-
Respiratory Changes: Breathing patterns often change, becoming irregular, shallow, or punctuated by periods of no breathing (Cheyne-Stokes respirations).
The Role of Medical Intervention and Palliative Care
It is crucial to understand that these thresholds often assume no further medical intervention.
-
In a Hospital Setting: Doctors may use supplemental oxygen or mechanical ventilation to support higher oxygen levels, even in end-of-life scenarios, for comfort.
-
In Palliative/Hospice Care: The focus may shift from aggressively treating numbers on a monitor to ensuring comfort and dignity, which sometimes means allowing natural physiological processes to occur without intervention.
The interpretation of these signs should always be done by healthcare professionals within the context of the patient's overall condition and goals of care.
Frequently Asked Questions (FAQ)
Q: Is an SpO2 of 70% a direct sign of imminent death?
A: While levels in the 70s are critically low and are commonly seen in the final days of life, they are not an immediate predictor of death within minutes or hours. It is a strong indicator that the body is shutting down, but the timeline varies greatly by individual and underlying condition.
Q: Should oxygen be given at the end of life?
A: This is a deeply personal decision made in consultation with the healthcare team and family. Supplemental oxygen can sometimes reduce the feeling of air hunger and provide comfort. However, for some, the discomfort of the equipment may not be worth the minimal benefit. This is a key discussion to have with hospice or palliative care providers.
Q: What matters more than the oxygen number itself?
A: The patient's comfort and symptoms matter most. Look for signs of distress like gasping, anxiety, or panic. Medical professionals are often less focused on the exact number and more focused on managing these symptoms to ensure peace and comfort.
Q: My loved one's oxygen is low but they seem peaceful. Should I be concerned?
A: In end-of-life care, peace and comfort are the primary goals. If the patient is not showing signs of distress (like agitation or gasping), a low oxygen level may be a natural part of the body's peaceful shutting down process. The clinical team can help you understand what to expect.
Disclaimer: This information is highly sensitive and is intended for educational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician, hospice nurse, or other qualified health provider with any questions you may have regarding a medical condition. The dying process is unique to each individual.