What Does "Source SpO2" Mean on a Hospital Monitor?
On a hospital vital signs monitor, "SpO2" or "Source SpO2" refers to the measurement of peripheral capillary oxygen saturation—the percentage of hemoglobin in your blood that is carrying oxygen. It is a non-invasive, real-time vital sign obtained from a sensor (usually on a finger) called a pulse oximeter.
The term "Source" indicates the specific input channel on the monitor where the SpO2 sensor is connected, distinguishing it from other monitored parameters like blood pressure or ECG.
How Source SpO2 is Measured: The Technology Behind the Number
The value is generated through a technology called pulse oximetry. Here’s how it works:
-
Light Emission: The sensor probe clipped to the patient's finger emits two wavelengths of light (red and infrared).
-
Light Absorption: Oxygenated hemoglobin (oxyhemoglobin) and deoxygenated hemoglobin absorb these two types of light differently.
-
Signal Detection: A photodetector on the other side of the probe captures the light that passes through the tissue.
-
Calculation: The monitor's internal computer calculates the ratio of absorbed red and infrared light to determine the percentage of oxygen-saturated hemoglobin, displaying it as the SpO2 value.
This entire process happens continuously, providing a second-by-second update on the patient's oxygenation status.
SpO2 vs. SaO2: What's the Difference?
It's crucial to understand this key distinction displayed on monitors:
| Feature | SpO2 | SaO2 |
|---|---|---|
| Method | Non-invasive (pulse oximetry) | Invasive (Arterial Blood Gas test) |
| Sample | Estimated via light through tissue | Direct measurement from an arterial blood draw |
| Accuracy | Estimated, with a ±2% margin of error | Gold standard, highly accurate |
| Use | Continuous monitoring | Intermittent, diagnostic snapshots |
⚡ Clinical Insight: SpO2 is invaluable for continuous trend monitoring, while SaO2 from an ABG test is used for definitive diagnosis and to measure exact blood gas levels.
Normal Range and Clinical Significance
-
Normal SpO2 Range: 95% to 100% for most healthy individuals.
-
Low (Hypoxemia): A reading below 90% is clinically significant and often triggers monitor alarms, indicating the patient may not be getting enough oxygen.
-
Individual Baselines: Patients with chronic lung diseases (e.g., COPD) may have a lower "normal" baseline (e.g., 88-92%) as determined by their pulmonologist.
Why is it so important? SpO2 is a primary indicator of respiratory function and tissue perfusion. A sudden drop can provide an early warning of respiratory distress or failure, allowing clinical staff to intervene quickly.
Factors That Can Affect Accuracy
Hospital staff are trained to recognize when an SpO2 reading might be unreliable. Key factors include:
-
Patient Motion: Shivering or restlessness can interfere with the signal.
-
Poor Perfusion: Low blood pressure, hypothermia, or vasoconstriction can make it difficult to get a strong signal.
-
Nail Polish & Artificial Nails: Especially dark colors can block light and skew results.
-
Skin Pigmentation: May affect accuracy, a known issue with some pulse oximetry technology.
-
Ambient Light: Bright overhead light can sometimes interfere with the sensor.
Frequently Asked Questions (FAQ)
Q: Why does my monitor sometimes show a weak signal or dashes (--)?
A: This typically means the monitor cannot detect a strong, pulsating blood flow. This is often due to cold hands, low blood pressure, or movement. Nurses will often reposition the sensor or warm the patient's hand to improve the signal.
Q: Is the hospital monitor more accurate than a home pulse oximeter?
A: Yes. Hospital monitors are higher-grade, regularly calibrated medical devices. While the core technology is the same, they are more sophisticated in filtering out motion artifact and providing reliable data in critical situations.
Q: What does the "pleth" or waveform next to the number mean?
A: That wavy line is the plethysmograph (or "pleth"). It represents the pulse volume at the sensor site. A strong, consistent wave confirms the SpO2 reading is based on a good pulse signal. A weak or flat line suggests poor perfusion or a misplaced sensor.
Q: Why is it called "Source" SpO2?
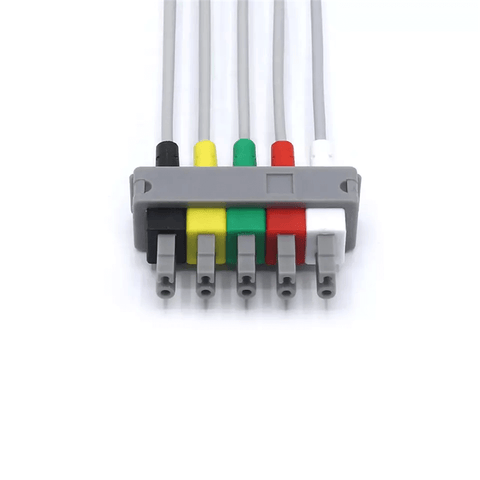
A: Modern monitors can display data from multiple sources (e.g., different SpO2 sensors, main monitor, wireless devices). "Source" specifies which connected device is providing that particular data stream.
Disclaimer: This information is for educational purposes only and is based on standard clinical practices. Patient care and the interpretation of monitor data are always managed by qualified healthcare professionals. Always rely on the advice of your medical team for diagnosis and treatment.