How to Read the Oxygen Level (SpO2) on a Hospital Monitor
If you're wondering how to read the oxygen level on a hospital vital signs monitor, you're likely checking on a loved one and want to understand what the numbers mean. This guide will help you quickly find the SpO2 reading and interpret it correctly.
The most important number to look for is labeled SpO2 (%), which stands for peripheral oxygen saturation. It's a percentage that measures how much oxygen your blood is carrying.

1. How to Find the SpO2 Reading on the Monitor
Hospital monitors can look complex, but finding the oxygen level is straightforward.
-
Look for "SpO2": Scan the display for the clear label "SpO2" or sometimes just "O2." It is almost always displayed next to a percentage number (%).
-
Identify the Number: The number next to it (e.g., 98%) is the current oxygen saturation level.
-
Find the Waveform: Often, there is a wavy line next to the number and a smaller number for the pulse rate. This wave shows the strength of the blood flow signal. A strong, consistent wave usually means a more accurate reading.
2. What Does the SpO2 Number Mean? Understanding the Values
The number itself is a percentage. Here’s what clinicians use as a general guide:
-
Normal Oxygen Level (95% to 100%): A reading in this range is typically considered normal and healthy for most individuals.
-
Low Oxygen Level (Hypoxemia): A consistent reading below 90% is generally considered low and is often called hypoxemia. This is typically when monitor alarms will activate to alert healthcare staff.
-
"Acceptable" Lower Levels (88-94%): It's crucial to know that for some patients with chronic lung conditions like COPD, a "normal" baseline might be lower (e.g., 88% to 92%) as determined by their doctor. This is why context from the care team is essential.
💡 Professional Context: While these ranges are standard, always rely on the healthcare team's assessment. They interpret the number in the context of the patient's overall condition, other vital signs, and medical history.
3. Key Factors That Affect the Reading's Accuracy
The number on the screen is an estimate. Its accuracy can be influenced by several factors:
-
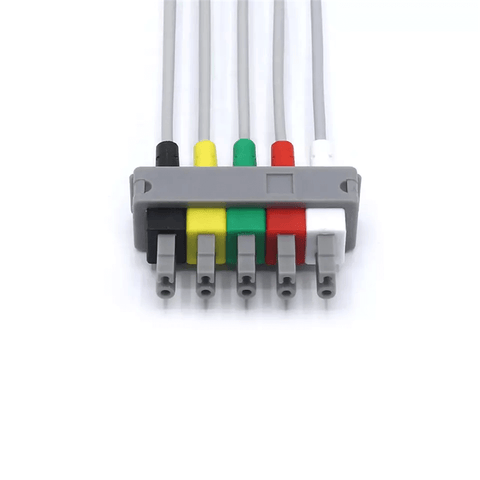
Sensor Placement: The clip-like sensor (a pulse oximeter) is usually on a finger. It must be clean, properly attached, and on a warm finger. Poor placement can cause inaccurate readings.
-
Patient Movement: Restlessness, shivering, or tremors can interfere with the sensor's ability to get a clear reading. The most accurate measurements are taken when the patient is still and calm.
-
Physical Characteristics: Nail polish (especially dark colors), artificial nails, very dark skin pigmentation, and poor circulation can sometimes affect accuracy. Clinical staff are trained to manage these factors.
-
Device Limitations: According to studies, standard pulse oximeters can have a margin of error of around 2% to 4%. Critical decisions are never based on this number alone.
4. Understanding Monitor Alarms
If the oxygen level drops below a preset threshold (often 90%), the monitor will trigger an alarm. This may be a beeping sound, the SpO2 number flashing, or a change in color. If an alarm sounds, stay calm and notify a nurse or healthcare professional. They are trained to assess the situation and determine if it's a true emergency or a minor issue (like a loose sensor).
Frequently Asked Questions (FAQ)
Q: What does a normal oxygen level look like on a hospital monitor?
A: A normal SpO2 reading for a healthy person at rest is typically between 95% and 100%. It will often be displayed in a neutral color like white or green.
Q: What should I do if the oxygen reading seems low or the alarm is going off?
A: The first and most important step is to alert a nurse or doctor immediately. Do not try to adjust the patient or the equipment yourself. They can check if the sensor is attached correctly and assess the patient directly.
Q: Why might the reading be inaccurate?
A: Common reasons for a falsely low reading include a cold finger, poor circulation, patient movement (shivering), or nail polish. The clinical team will check for these issues if a reading seems unexpected.
Q: Is the pulse oximeter reading the same as an blood oxygen test?
A: No. The monitor uses a non-invasive estimate (SpO2). A more precise measurement requires an arterial blood gas (ABG) test, which draws blood and measures oxygen directly (PaO2). The SpO2 is used for continuous, non-invasive monitoring.
Disclaimer: This guide is for informational purposes to help you understand hospital equipment. It is not medical advice. Always rely on the interpretations and guidance of the attending healthcare professionals.